Society Guidelines
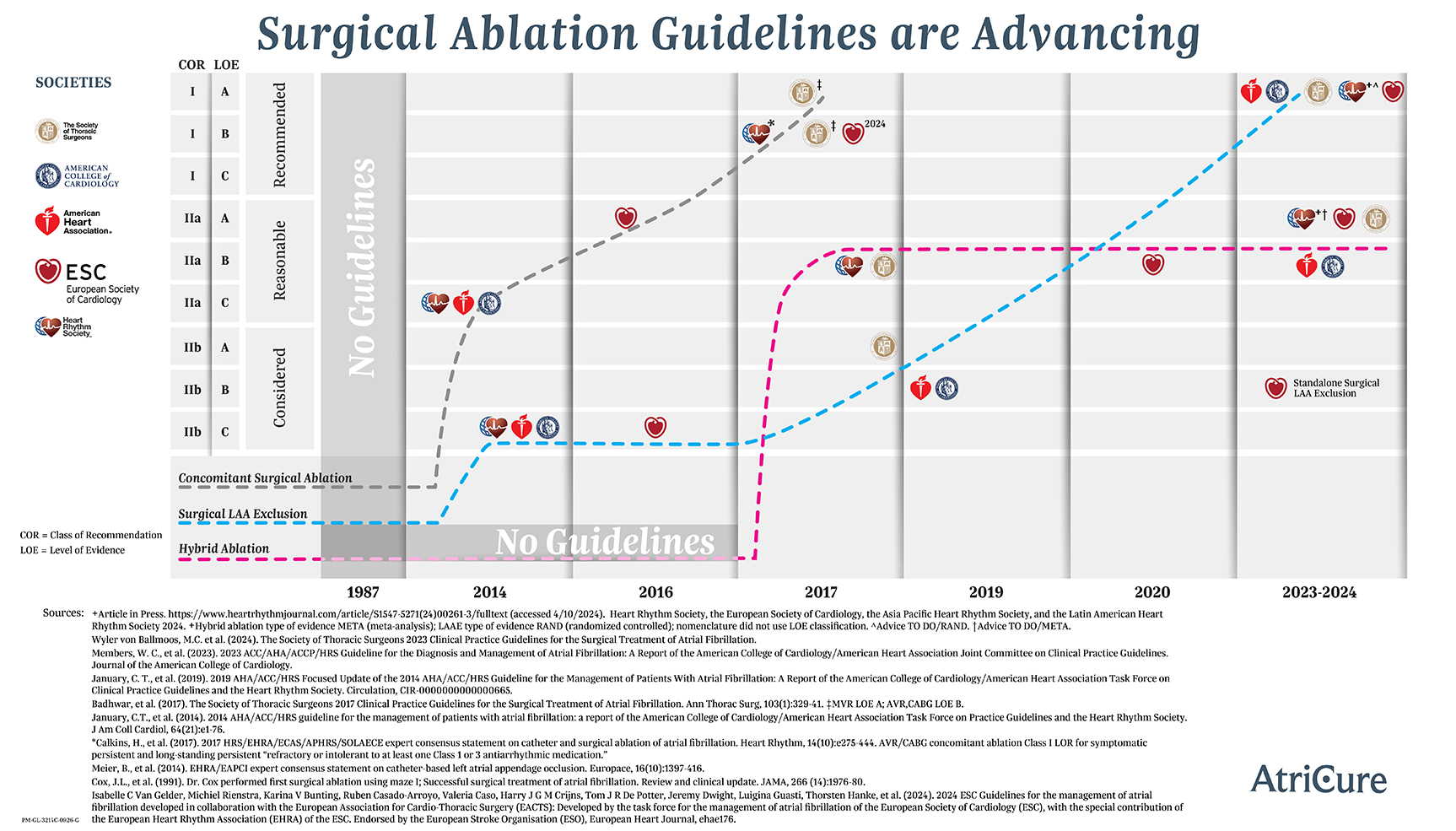
For Treatment of Atrial Fibrillation (Afib or AF)
| Society | Recommendation |
| ACC/AHA/ACCP/HRS (2023)1 | For patients with AF who are undergoing cardiac surgery, concomitant surgical ablation can be beneficial to reduce the risk of recurrent AF (Class IIa, Level B-R) In patients undergoing surgical ablation, anticoagulation therapy is reasonable for at least 3 months after the procedure to reduce the risk of stroke or systemic embolism. (Class IIa, Level B-NR) For patients with symptomatic, persistent AF refractory to antiarrhythmic drug therapy, a hybrid epicardial and endocardial ablation might be reasonable to reduce the risk of recurrent atrial arrhythmia (Class IIb, Level B-R) “Among patients with symptomatic, persistent AF, a hybrid procedure combining epicardial and endocardial ablation has been shown to reduce the burden of atrial arrhythmia." |
| STS (2017)2 | “Surgical ablation for AF can be performed without additional risk of operative mortality or major morbidity and is RECOMMENDED at the time of concomitant mitral operations to restore sinus rhythm. (Class I, Level A)” “Surgical ablation for AF can be performed without additional operative risk of mortality or major morbidity, and is RECOMMENDED at the time of concomitant isolated aortic valve replacement, isolated coronary artery bypass graft surgery, and aortic valve replacement plus coronary artery bypass graft operations to restore sinus rhythm. (Class I, Level B nonrandomized)” “In the treatment of AF, multidisciplinary heart team assessment, treatment planning, and long-term follow-up can be USEFUL AND BENEFICIAL to optimize patient outcomes. (Class I, Level C expert opinion)” “Surgical ablation for symptomatic AF in the absence of structural heart disease that is refractory to Class I/III antiarrhythmic drugs or catheter-based therapy or both is REASONABLE as a primary stand-alone procedure, to restore sinus rhythm. (Class IIa, Level B randomized)” “Surgical ablation for symptomatic persistent or longstanding persistent AF in the absence of structural heart disease is REASONABLE, as a stand-alone procedure using the Cox-Maze III/IV lesion set compared with pulmonary vein isolation alone. (Class IIa, Level B nonrandomized)” |
| HRS/EHRA/ECAS/ APHRS/SOLAECE (2017)3 | “Surgical ablation of AF is recommended for paroxysmal, persistent, and long-standing persistent patients who are symptomatic AF refractory or intolerant to at least one Class I or III antiarrhythmic medication during concomitant open procedures (such as MVR). (Class I, Level B nonrandomized)” “Surgical ablation of AF is recommended for paroxysmal, persistent, and long-standing persistent patients who are symptomatic AF prior to initiation of antiarrhythmic therapy with a Class I or III antiarrhythmic medication during concomitant open procedures (such as MVR). (Class I, Level B nonrandomized)” “Surgical ablation of AF is recommended for paroxysmal, persistent, and long-standing persistent patients who are symptomatic AF refractory or intolerant to at least one Class I or III antiarrhythmic medication during concomitant closed procedures (such as CABG and AVR). (Class I, Level B nonrandomized)” “Surgical ablation of AF is reasonable for paroxysmal, persistent, and long-standing persistent patients who are symptomatic AF prior to initiation of antiarrhythmic therapy with a Class I or III antiarrhythmic medication during concomitant closed procedures (such as CABG and AVR). (Class IIa, Level B nonrandomized)” “Stand-Alone and Hybrid surgical ablation of AF is reasonable for persistent, and long-standing persistent patients who are symptomatic AF refractory or intolerant to at least one Class I or III antiarrhythmic medication and have failed one or more attempts at catheter ablation or prefer a surgical approach. (Class IIa, Level B nonrandomized)” “Stand-Alone and Hybrid surgical ablation of AF can be considered for paroxysmal patients who are symptomatic AF refractory or intolerant to at least one Class I or III antiarrhythmic medication and have failed one or more attempts at catheter ablation or prefer a surgical approach. (Class IIb, Level B nonrandomized)” |
| AATS (2017)12 | “It is recommended to choose to perform a concomitant surgical ablation procedure for patients with a history of AF over no treatment of AF because there is a significant improvement in operative survival associated with surgical ablation. (Class I, LOE A)” “It is reasonable to choose to perform a concomitant surgical ablation procedure for patients with a history of AF over no treatment of AF because long-term survival is unaffected or improved by surgical ablation. (Class IIa)
“It is reasonable to choose to perform a concomitant surgical ablation procedure for patients with a history of AF over no treatment of AF because there is no increased risk of perioperative stroke/TIA (Class IIa, LOE A)” “It is reasonable to choose to perform a concomitant surgical ablation procedure for patients with a history of AF over no treatment of AF because the incidence of late stroke/TIA is unaffected or decreased by surgical ablation. (Class IIa)
“It is reasonable to choose to perform a concomitant surgical ablation procedure for patients with a history of AF over no treatment of AF because the incidence of perioperative morbidity is not increased by surgical ablation. (Class IIa)
“It is reasonable to choose to perform a concomitant surgical ablation procedure for patients with a history of AF over no treatment of AF because there is a significant improvement in [health related quality of life] (HRQL) and AF-related symptoms associated with surgical ablation of AF. (Class IIa)
“Hybrid procedures may be considered as a stand-alone procedure in patients with appropriate indications and by an experienced heart team. (Class IIb, LOE B-NR)” “It is reasonable to perform stand-alone surgical ablation for pulmonary vein isolation in patients with symptomatic paroxysmal AF and small left atria. (Class IIa, LOE B-R)” “The best evidence exists for the use of bipolar radiofrequency clamps and cryoablation devices, which have become integral parts of many procedures, including pulmonary vein isolation and the Cox-Maze IV procedure. The use of epicardial unipolar RF ablation outside of clinical trials is not recommended, because its efficacy remains questionable. “Training and education should be considered before the performance of surgical ablation, but the effectiveness of the training program is unclear. More specific research needs to be conducted because there have been limited populations evaluated. (Class I, LOE C)” |
| ISMICS (2009)4 | “Concomitant surgical ablation is recommended …. to increase the incidence of sinus rhythm both at short- and long-term follow-up …. to improve ejection fraction and exercise tolerance …. to reduce the risk of stroke and thromboembolic events …. and to improve long-term survival.” |
| UK NICE (2014)5 | "Surgical ablation of AF should be considered in patients with persistent AF, or with symptomatic AF undergoing cardiothoracic surgery." |
| ESC (2010)6 | "Surgical ablation of AF should be considered in patients with symptomatic or asymptomatic AF undergoing cardiac surgery." "Minimally invasive surgical ablation of AF without concomitant cardiac surgery is feasible and may be performed in patients with symptomatic AF after failure of catheter ablation." |
For Left Atrial Appendage Management (LAAM)
| Society | Recommendation |
| STS (2024)13 | “Left atrial appendage obliteration for atrial fibrillation is recommended for all first-time non-emergent cardiac surgery procedures, with or without concomitant surgical ablation, to reduce morbidity from thromboembolic complications. (Class Ia)” |
| ACC/AHA/ACCP/HRS (2023)1 | In patients with AF undergoing cardiac surgery with a CHA2DS2-VASc score of ≥2 or equivalent stroke risk, surgical LAA exclusion, in addition to continued anticoagulation, is indicated to reduce the risk of stroke and systemic embolism (Class I, Level A) In patients with AF undergoing cardiac surgery and LAA exclusion, a surgical technique resulting in absence of flow across the suture line and a stump of <1 cm as determined by intraoperative transesophageal echocardiography should be used. (Class I, Level A) In patients with AF undergoing cardiac surgery with a CHA2DS2-VASc score of ≥2 or equivalent stroke risk, the benefit of surgical LAA exclusion in the absence of continued anticoagulation to reduce the risk of stroke and systemic embolism in uncertain. (Class IIb, Level A) |
| UK NICE (2014)8 | "Consider LAA occlusion if anticoagulation is contraindicated or not tolerated and discuss the benefits and risks of LAAO with patient." |
| EJCTS (2013)9 | "We conclude that there has been no proven benefit of surgical LAA exclusion in terms of stroke reduction or mortality benefit… If exclusion is contemplated, devices designed for appendage exclusion should be used rather than a cut-and-sew or stapling technique." |
| EHRA/EAPCI10,11 | "OAC (with VKA or NOACs) is the standard therapy; however, for patients who are contraindicated or refuse (N) OACs… the main indication for LAA occlusion is a relative or absolute contraindication to (N)OACs in patients with AF and a CHADS2 score of ≥1 or CHA2 -DS2 -VASc score ≥ 2." |
- Jogler JA et al. 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2023 Nov 30. doi: 10.1161/CIR.0000000000001193
- Vinay Badhwar, J. Scott Rankin, Ralph J. Damiano, A. Marc Gillinov, Faisal G. Bakaeen, James R. Edgerton, Jonathan M. Philpott, Patrick M. McCarthy, Steven F. Bolling, Harold G. Roberts, Vinod H. Thourani, Rakesh M. Suri, Richard J. Shemin, Scott Firestone, Niv Ad. The Society of Thoracic Surgeons 2017 Clinical Practice Guidelines for the Surgical Treatment of Atrial Fibrillation. The Annals of Thoracic Surgery, 2017; 103: 329-41.
- Calkins H, Hindricks G, Cappato R, Kim Y-H, Saad EB, Aguinaga L, Akar JG, Badhwar V, Brugada J, Camm J, Chen P-S, Chen S-A, Chung MK, Nielsen JC, Curtis AB, Davies DW, Day JD, d’Avila A, (Natasja) de Groot NMS, Di Biase L, Duytschaever M, Edgerton JR, Ellenbogen KA, Ellinor PT, Ernst S, Fenelon G, Gerstenfeld EP, Haines DE, Haissaguerre M, Helm RH, Hylek E, Jackman WM, Jalife J, Kalman JM, Kautzner J, Kottkamp H, Kuck KH, Kumagai K, Lee R, Lewalter T, Lindsay BD, Macle L, Mansour M, Marchlinski FE, Michaud GF, Nakagawa H, Natale A, Nattel S, Okumura K, Packer D, Pokushalov E, Reynolds MR, Sanders P, Scanavacca M, Schilling R, Tondo C, Tsao H-M, Verma A, Wilber DJ, Yamane T, 2017 HRS/EHRA/ECAS/APHRS/SOLAECE Expert Consensus Statement on Catheter and Surgical Ablation of Atrial Fibrillation, Heart Rhythm (2017), doi: 10.1016/j.hrthm. 2017.05.012.
- Ad et al.; Surgical ablation for atrial fibrillation in cardiac surgery. Innovations, vol 5, no 2, March/April 2010.
- National Institute for Health and Care Excellence. Atrial fibrillation: management, clinical guideline. June 18, 2014.
- Camm et al.; Guidelines for the management of atrial fibrillation. European Heart Journal, 2010.
- January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland Jr JC, Ellinor PT, Ezekowitz MD, Field ME, Furie KL, Heindenreich PA, Murray KT, Shea JB, Tracy CM, Yancy CW, 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guidelines for the Management of Patients With Atrial Fibrillation, Journal of the American College of Cardiology (2019), doi: https://doi.org/10.1016/j.jacc.2019.01.011.
- National Institute for Health and Care Excellence. Atrial fibrillation: management, clinical guideline. June 18, 2014.
- Dunning et al.; Guideline for the surgical treatment of atrial fibrillation. European Journal of Cardio-Thoracic Surgery. Vol 44. 2013.
- Meier et al.; EHRA/EAPCI expert consensus statement on catheter-based left atrial appendage occlusion. EuroIntervention. 2014
- Thambo et al.; The future of left atrial appendage occlusions: When extraordinary claims require evidence… Archives of Cardiovascular Disease 2015 vol 108.
- Ad N, et al, Expert consensus guidelines: Examining surgical ablation for atrial fibrillation, J Thorac Cardiovasc Surg, 2017 Jun;153(6):1330-1354.
- Wyler von Ballmoos, M.C. et al. (2024). The Society of Thoracic Surgeons 2023 Clinical Practice Guidelines for the Surgical Treatment of Atrial Fibrillation.

